Tele-behavioral health has become a preferred mode of care delivery for many mental health practices. Patients benefit from accessibility, while providers gain flexibility in scheduling and care continuity.
However, billing tele-behavioral Health Services correctly is not always straightforward. Small errors in place of service selection, modifier usage, or documentation can lead to avoidable denials and delayed payments.
This guide walks through tele-behavioral health billing using real-world scenarios, sample coding examples, and payer-specific considerations to help practices submit clean and compliant claims.
SCENARIO 1: VIDEO THERAPY SESSION WITH A COMMERCIAL PAYER
Scenario
A licensed therapist conducts a 45-minute psychotherapy session via video with an established patient who has a commercial insurance plan.
Commonly billed service
Psychotherapy, 45 minutes
Sample billing structure
CPT Code: 90834
Place of Service: POS based on payer guidelines
Modifier: Telehealth modifier as required by the payer
Common mistake
Using an in-office POS without a telehealth modifier, or using a telehealth POS when the payer expects the office POS with a modifier.
Why this gets denied
Commercial payers differ widely in how they want tele-behavioral health services billed. Some expect the POS to reflect where the provider would have been located if the service were in person, while others require a telehealth-specific POS.
Best practice
Always verify payer-specific telehealth billing rules before submitting claims and apply the POS and modifier consistently.
PLACE OF SERVICE CODES IN TELE-BEHAVIORAL HEALTH
Place of service selection tells the payer where the service occurred and directly affects reimbursement.
Common POS considerations in tele-behavioral health include:
• Office-based POS when billing as if the service were in person
• Telehealth-specific POS when required by the payer
• Avoiding POS and modifier mismatches
Incorrect POS usage is one of the most frequent causes of tele-behavioral health claim rejections.
SCENARIO 2: MEDICARE TELE-BEHAVIORAL HEALTH VISIT
Scenario
A psychiatrist provides a follow-up medication management visit via telehealth to a Medicare patient.
Commonly billed service
Medication management or evaluation and management service
Sample billing structure
CPT Code: Based on the service level documented
Place of Service: POS per Medicare telehealth guidance
Modifier: Telehealth modifier as required
Common mistake
Billing Medicare telehealth visits using commercial payer rules or missing required telehealth indicators.
Why this gets denied
Medicare tele-behavioral health rules differ from commercial plans and may change year over year. Claims are often denied when practices assume the same rules apply across payers.Best practice
Maintain a Medicare-specific tele-behavioral health billing checklist and review updates regularly.
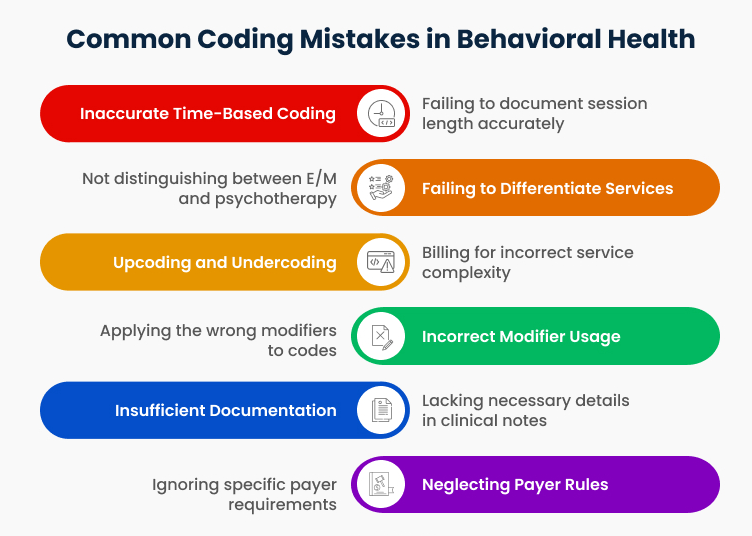
TELEHEALTH MODIFIERS IN BEHAVIORAL HEALTH BILLING
Modifiers indicate that services were delivered remotely and play a key role in tele-behavioral health billing.
Common issues include:
• Missing telehealth modifiers
• Using a modifier not accepted by the payer
• Applying different modifiers inconsistently across claims
These errors can result in denials even when the CPT code itself is correct.
SCENARIO 3: AUDIO-ONLY TELE-BEHAVIORAL HEALTH VISIT
Scenario
A therapist conducts a behavioral health session via phone due to the patient lacking video access.
Common challenge
Not all payers reimburse audio-only behavioral health services.
Sample billing considerations
• Verify whether the payer allows audio-only visits
• Confirm approved CPT codes for audio-only services
• Ensure documentation clearly supports the service modality
Common mistake
Billing audio-only visits the same way as video telehealth visits.
Why this gets denied
Many payers require explicit indicators that the visit was audio-only and may restrict coverage based on patient location or diagnosis.
Best practice
Document the reason for audio-only care and verify payer coverage before billing.
DOCUMENTATION AND COMPLIANCE REQUIREMENTS
Strong documentation is the backbone of compliant tele-behavioral health billing.
Documentation should clearly include:
• Patient consent for telehealth
• Service modality used
• Patient and provider locations
• Start and end time when required
• Clinical notes supporting medical necessity
Missing documentation is a common trigger for audits and post-payment reviews.
COMMON TELE-BEHAVIORAL HEALTH DENIALS
Based on billing trends, the most frequent tele-behavioral health denials occur due to:
• Incorrect POS and modifier combinations
• Provider not credentialed for telehealth
• Services not covered under payer telehealth policy
• Missing consent or incomplete documentation
These denials are preventable with standardized workflows.
BEST PRACTICES FOR TELE-BEHAVIORAL HEALTH BILLING
To reduce denials and improve reimbursement, practices should:
• Maintain payer-specific telehealth billing guidelines
• Use standardized tele-behavioral health documentation templates
• Verify credentialing and enrollment for telehealth services
• Audit telehealth claims regularly
• Partner with billing teams experienced in behavioral health telehealth workflows
CONCLUSION
Tele-behavioral Health Billing is not just about choosing the right CPT code. It requires careful coordination between clinical documentation, coding accuracy, payer rules, and compliance requirements.
By understanding real-world billing scenarios and applying payer-specific guidelines, behavioral health practices can reduce denials, improve cash flow, and deliver care confidently through telehealth.
Acuity Health Solutions supports behavioral health practices with tele-behavioral health billing, credentialing, and compliance-driven revenue cycle management. Our team helps practices navigate payer rules with confidence and consistency.