As healthcare enters 2026, automation is no longer an enhancement to revenue cycle management. It is a requirement. Providers that continue to rely on manual billing workflows will face rising denials, slower reimbursements, and increased compliance risk.
In this blog, we outline how technology and automation are transforming healthcare billing, which RCM functions benefit the most, and how providers should structure their automation strategy going into 2026.
Why 2026 Is a Turning Point for RCM
The healthcare billing landscape has changed permanently. Increasing payer scrutiny, evolving CMS regulations, and ongoing staffing challenges have made traditional RCM models unsustainable.
By 2026, successful healthcare organizations will share three traits:
- Digitally automated front-end workflows
- Intelligent, rules-driven claims processing
- Real-time financial and operational visibility
Automation is no longer about speed alone. It is about accuracy, predictability, and compliance at scale.
The Evolution of RCM: From Manual to Intelligent Automation
Legacy RCM workflows typically involve:
- Manual eligibility verification
- Post-visit coding and charge entry
- Reactive denial handling
- Delayed AR and cash reporting
Modern RCM automation replaces these with proactive, data-driven processes that reduce errors before claims ever reach a payer.
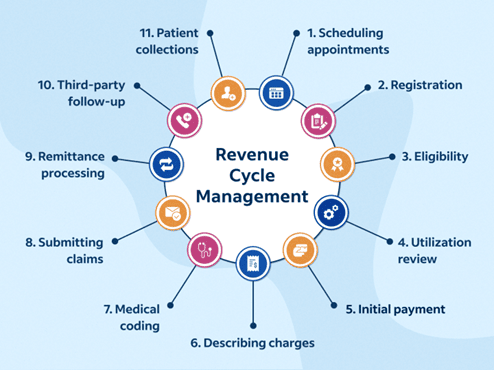
Key Areas of Automation in Healthcare Billing and RCM
Automated Eligibility and Benefits Verification
Eligibility-related errors remain one of the highest contributors to claim denials. Automation enables real-time verification during scheduling and check-in.
Automation capabilities include:
- Instant confirmation of active coverage
- Identification of authorization and referral requirements
- Accurate calculation of patient responsibility
Impact:
- Fewer front-end errors
- Improved patient collections
- Reduced downstream rework
AI-Assisted Medical Coding and Charge Capture
AI-powered coding tools analyze clinical documentation and suggest compliant CPT, ICD-10, and modifier combinations based on payer-specific logic.
Key advantages:
- Reduced undercoding and overcoding risk
- Faster charge capture turnaround
- Better alignment with payer and CMS guidelines
AI enhances certified coders by handling repetitive patterns while allowing human review for complex encounters.
Intelligent Claim Scrubbing and Pre-Submission Validation
Modern RCM platforms apply payer-specific edits before claims are submitted.
Pre-submission checks include:
- NCCI and modifier validation
- Local coverage determinations
- Missing or inconsistent data detection
Business impact:
Higher first-pass acceptance rates
Lower denial volumes
Reduced billing team workload
Automated Denial Management and Work Queues
Advanced denial automation supports:
- Auto-correction and resubmission of common errors
- Prioritization based on claim value
- Trend analysis by payer, CPT, and location
Result:
Faster recovery of lost revenue
Better payer negotiation insights
Lower AR days
Real-Time RCM Dashboards and Analytics
By 2026, static monthly reports will be obsolete. Automated RCM relies on real-time dashboards.
Key metrics tracked include:
- Days in AR
- First-pass resolution rate
- Denial rate by payer and specialty
- Net collection percentage
Leadership gains immediate visibility into financial performance and operational bottlenecks.
Role of Health IT Integration in RCM Automation
Automation is only effective when billing systems integrate seamlessly with EHRs, clearinghouses, and payer portals.
Strong integration enables:
- Clean data flow from clinical documentation to claims
- Automated ERA and patient payment posting
- Consistent audit trails for compliance
Fragmented systems introduce manual workarounds that weaken automation outcomes.
Compliance and Security Considerations for Automated RCM
Automation must align with regulatory and security requirements.
Key compliance priorities include:
- HIPAA privacy and security safeguards
- CMS billing and documentation standards
- Role-based access and audit logging
Well-designed automation reduces compliance risk by enforcing standardized workflows and minimizing manual intervention.
What Healthcare Organizations Should Prioritize for 2026
Providers planning their RCM roadmap for 2026 should focus on practical automation that delivers measurable outcomes.
Recommended priorities:
- Front-end automation before back-end cleanup
- Specialty-Specific Billing logic
- Embedded payer-rule intelligence
- Actionable reporting tied to revenue performance
Technology should simplify workflows, not add operational complexity.
How Acuity Health Approaches Technology-Driven RCM
At Acuity Health, automation is implemented as part of a broader operational strategy, not as a standalone tool.
Our approach focuses on:
- Identifying revenue leakage points
- Aligning technology with specialty-specific workflows
- Implementing automation without disrupting day-to-day operations
- Maintaining compliance while scaling efficiently
The goal is consistent, predictable revenue performance
Conclusion: Preparing for the Future of RCM
As healthcare moves into 2026, automation will define the difference between stable revenue cycles and constant financial firefighting.
Organizations that invest in intelligent RCM technology, integrated Health IT systems, and expert oversight will be best positioned to navigate payer complexity and regulatory change.
The future of Healthcare Billing is automated, data-driven, and proactive.