Artificial Intelligence is becoming deeply embedded in medical coding workflows, but not all AI solutions deliver the same value. As we move into 2026, providers must separate practical, compliance-ready AI tools from overhyped promises of fully autonomous coding.
This blog explains how AI is actually being used in medical coding today, where it delivers measurable ROI, where human expertise remains critical, and how Healthcare Organizations should adopt AI-assisted coding responsibly.
Why AI in Medical Coding Matters in 2026
Medical coding sits at the intersection of clinical care, compliance, and revenue. Increasing documentation complexity, frequent payer rule changes, and staffing shortages have made traditional coding models difficult to sustain.
AI has emerged as a powerful support layer, helping coding teams process higher volumes with greater consistency. However, unrealistic expectations around “fully automated coding” have also created confusion in the market.
In 2026, success lies in augmentation, not replacement.
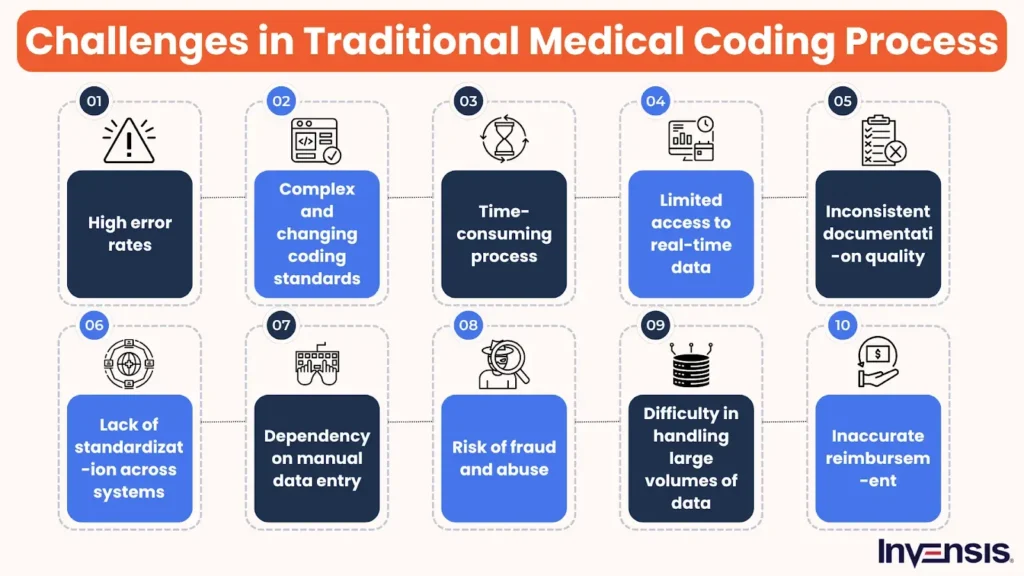
The Reality of Medical Coding Challenges
Before understanding AI’s role, it’s important to recognize the current pain points in coding operations.
Common challenges include:
- High chart volumes and turnaround pressure
- Inconsistent documentation quality
- Payer-specific coding and modifier rules
- Risk of undercoding, overcoding, and audits
- Burnout among certified coders
AI addresses some of these challenges, but not all.
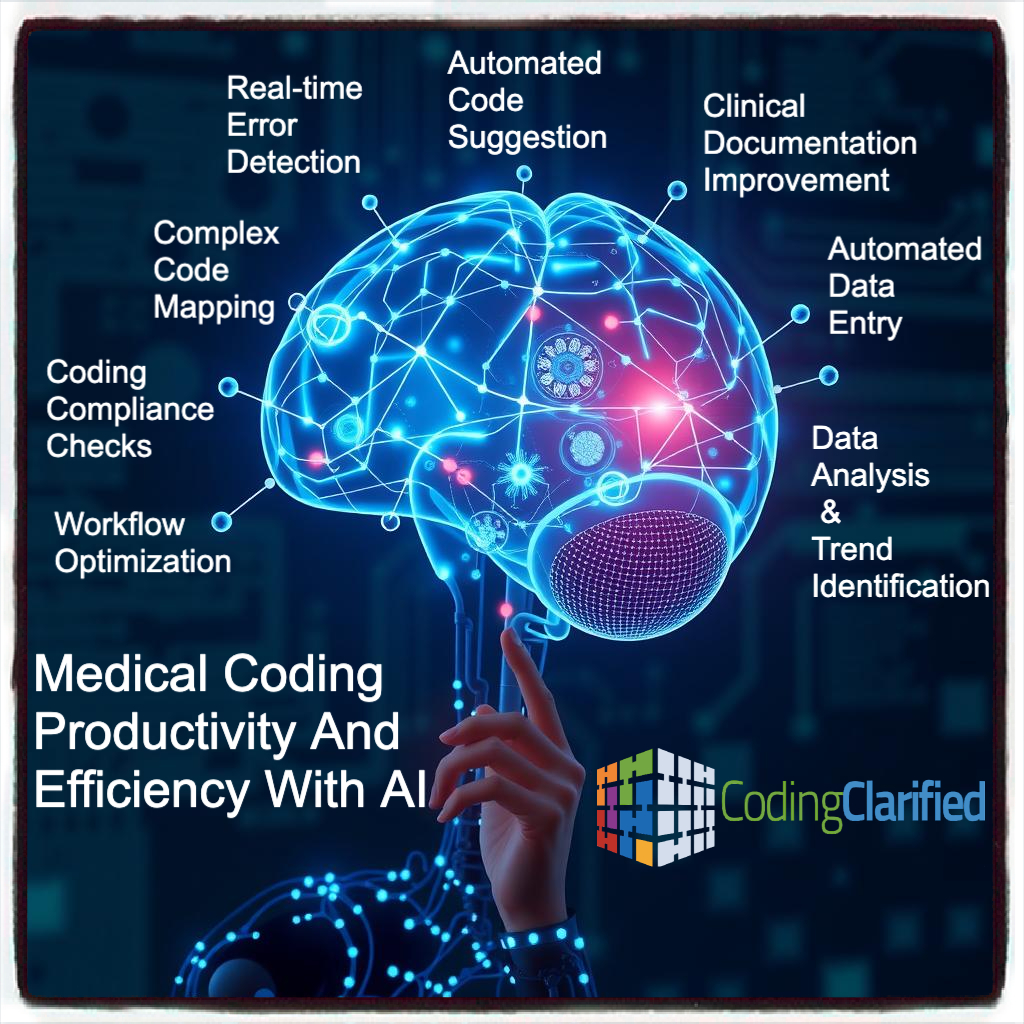
What AI in Medical Coding Actually Does Well
AI-powered coding tools use natural language processing and machine learning to analyze clinical documentation and identify relevant coding elements.
Core capabilities include:
- Identifying likely CPT and ICD-10 codes from documentation
- Flagging missing or unclear documentation
- Suggesting appropriate modifiers based on encounter context
- Applying payer and specialty-specific coding logic
These tools excel at pattern recognition across large datasets, making them ideal for repetitive and rules-driven coding scenarios.
Where AI Delivers Real Value in Coding Workflows
1. Faster Charge Capture
AI significantly reduces the time between clinical documentation completion and charge entry.
Impact:
- Shorter billing cycles
- Earlier claim submission
- Improved cash flow predictability
2. Improved Coding Consistency
AI applies the same logic across charts, reducing variability caused by fatigue or subjective interpretation.
Impact:
- More consistent coding outcomes
- Reduced internal rework
- Better audit defensibility
3. Documentation Gap Identification
AI tools highlight missing elements such as laterality, medical necessity indicators, or incomplete procedure descriptions.
Impact:
- Cleaner claims
- Fewer payer rejections
- Improved provider documentation habits
Where the Hype Falls Apart
Despite marketing claims, AI cannot fully replace human coders in 2026.
Limitations include:
- Inability to interpret nuanced clinical intent
- Difficulty handling complex, multi-procedure encounters
- Limited understanding of payer-specific gray areas
- Inability to assume compliance liability
AI lacks clinical judgment and contextual awareness. Final coding responsibility must remain with trained professionals.
The Role of Human Coders in an AI-Enabled Model
In an effective AI-assisted coding workflow, human coders transition from data entry to oversight and decision-making roles.
Human expertise remains essential for:
- Complex surgical and specialty coding
- Modifier strategy and payer appeal scenarios
- Audit preparation and compliance reviews
- Edge cases and evolving payer rules
AI increases coder productivity, but human validation ensures accuracy and compliance.
Compliance and Risk Considerations
AI-assisted coding must align with regulatory expectations.
Key compliance principles include:
- Clear audit trails showing human review
- Documented coding policies and escalation paths
- Role-based access and approval workflows
- Regular validation of AI outputs
Providers remain responsible for claims accuracy, regardless of automation level.
How Providers Should Adopt AI Coding in 2026
Successful adoption requires a phased, realistic approach.
Recommended steps:
- Start with high-volume, low-complexity encounters
- Use AI as a recommendation engine, not an auto-submit tool
- Maintain coder review and sign-off
- Continuously monitor denial and audit trends
AI should be integrated into existing RCM workflows rather than deployed as a standalone solution.
How AI Fits Into the Broader RCM Automation Strategy
AI-assisted coding is most effective when combined with:
- Automated eligibility verification
- Pre-submission claim validation
- Denial trend analytics
- Integrated EHR and billing platforms
Isolated AI tools provide limited value without end-to-end revenue cycle alignment.
How Acuity Health Approaches AI-Assisted Coding
At Acuity Health, AI is used to enhance accuracy and efficiency while maintaining full compliance oversight.
Our approach focuses on:
- Specialty-specific AI configuration
- Human-in-the-loop validation models
- Alignment with payer and CMS requirements
- Continuous performance monitoring
We prioritize sustainable revenue outcomes over experimental automation.
Conclusion: AI Is a Tool, Not a Shortcut
In 2026, AI in medical coding is neither a silver bullet nor a passing trend. It is a powerful tool when applied thoughtfully and responsibly.
Healthcare organizations that view AI as an enhancement to expert-driven workflows will see improvements in speed, accuracy, and compliance. Those chasing full automation without oversight risk revenue loss and regulatory exposure.
The future of Medical Coding is collaborative: intelligent systems guided by experienced professionals.