One of the most complicated fields of Revenue Cycle Management is infusion therapy billing. Even small coding or documentation mistakes can easily result in denials, underpayment, or payer audit. In the case of hospitals, infusion centers, and specialty practices, it is essential to understand the rules of CPT coding, the modifiers to use, and audit risks to ensure that revenue is not lost and that practices are compliant.
This guide summarizes the basic billing guidelines that providers should use to ensure accurate and consistent billing of infusion services.
Understanding Infusion Therapy Billing Basics
The billing of infusion therapy follows largely the CPT codes 96360-96379 dealing with billing and infusion therapy; hydration, therapeutic, prophylactic, and diagnostic infusions, in addition to injections. Instead of a drug being administered, coding is done based on time, purpose of the service, and route of administration.
Payers are demanding good compliance with National Correct Coding Initiative (NCCI) edits, Medicare, and payer-specific policies. Mistakes in documentation or charge capture are usually revealed in audits several months later, and it is therefore essential to be proactive for accurate results.
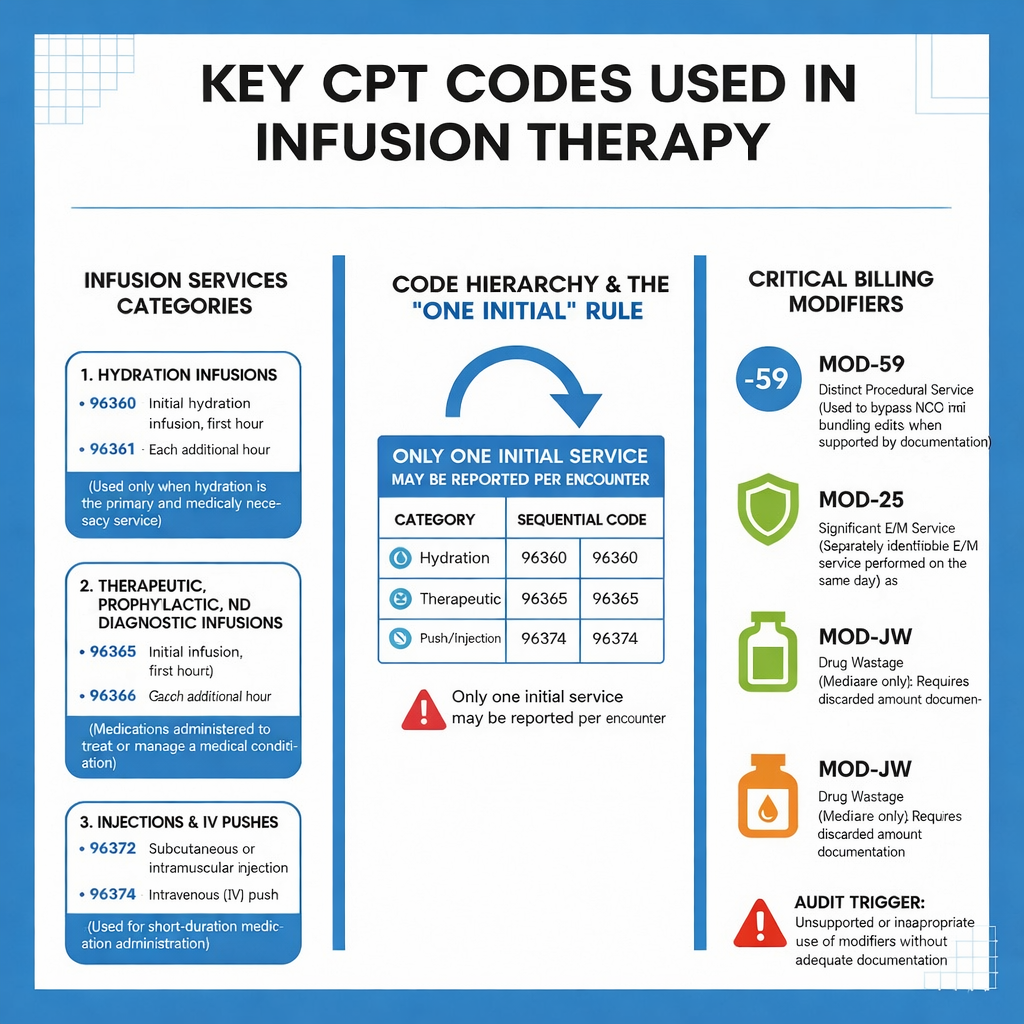
Key CPT Codes Used in Infusion Therapy
Infusion services can be divided into the three major categories:
Hydration Infusions
The 96360 (first hydration, not exceeding one hour) and 96361 (follow-up hydration, one hour after the first one) are only applicable when the primary cause of the encounter is hydration and is medically necessary.
Since the early 1960s and continuing to the present, various therapeutic, prophylactic, and diagnostic infusions have been created and developed (Desmond, 2013).
Such codes as 96365 (first infusion, not exceeding 1 hour) and 96366 (one hour later) are applied in case the medications are used to treat or manage a condition.
Injections and Pushes
Such codes as 96372 (subcutaneous or intramuscular injection) and 96374 (IV push) are used when the time of medication delivery is not supportive of infusion time limits.
There is only a single initial service that can be charged in case many drugs are given during a single encounter.
Modifier Usage in Infusion Billing
Modifiers are also very important when it comes to proper billing of infusion:
The use of modifier -59 to denote a discrete service is a procedural service in case of NCCI edits; services would be bundled together. It should be backed with effective documentation.
Modifier- 25 could be used in cases where there is substantial, distinctly identifiable E/M service on the same day, in which case the infusion therapy was carried out.
When the discarded amounts of drugs are recorded and reported accordingly, then they are billed with the modifier -JW when related to Medicare.
One frequent audit trigger is the use or misuse of modifiers where there is no obvious documentation to support medical necessity or separateness.
Documentation Requirements Payers Expect
The correct infusion billing requires accurate documentation, which includes:
- Initial and final times of every infusion.
- Name of drug, dosage, and route of intake.
- Clinical intent and medical necessity.
- Continuous infusion Nursing notes.
- Missing or estimated times are also a common reason behind downcoding/denial.
Common Audit Risks in Infusion Therapy Billing
The high reimbursement and complexity of infusion services render them prone to audit. Common audit risks include:
- Billing hydration as incidental to another infusion.
- Wrongful choice of first vs. second service.
- Unsupported modifier usage
- Infusion time is below the minimum.
- Abnormal drug unit-administration code mismatch.
- Patterns that payers also examine equally are the routine use of high-level infusion codes or the overutilization of modifier -59.
How Acuity Health Solutions Supports Infusion Billing Accuracy
Acuity Health Solutions assists the providers in reducing the infusion billing risk by considering the payer-aligned code, documentation audits, and preventing denials.
With front-end editing and applying existing CPT guidelines, NCCI edits, and payer-specific rules, Acuity exposes the audit to a minimum, and it also enhances first-pass claims acceptance.